A new strain of Mpox has been found outside its country of origin but a health expert here says there’s no need for Kiwis to panic.
The World Health Organization has declared the outbreak of Mpox Clade 1 in Central Africa a public health emergency of international concern.
Health experts believe it’s more transmissible and more severe than the Clade 2 strain that’s already spread globally.
So far 96 percent of the cases are in the Democratic Republic of Congo, but infection is spreading rapidly in neighbouring countries. Two cases have been detected in Pakistan, and one in the Philippines. On Thursday Sweden reported its first case, and its health agency confirmed the person contracted the virus during a recent stay in Africa and is now isolating.
It sounds alarming but an infectious disease expert from the University of Auckland says we don’t need to be stockpiling toilet paper just yet.
New Zealanders should be keeping an eye on how the outbreak develops but Associate Professor Mark Thomas thinks it will be some time before it gets here.
※It won’t be an overwhelming number of cases to begin with and likely public health efforts assisted by vaccination will bring it under control relatively quickly. By that, I would think within a month or two,§ he says.
The main point of concern is the severity of Clade 1, and its higher death rate which is 10 percent. The other variant is found in West Africa and has a lower death rate of about 1 percent.
But those death rates are based on case and death figures from the African countries where the virus originates.
Thomas says during the last global spread of Mpox Clade 2 a couple of years ago, other countries didn’t record the same mortality rates.
And that could be for several reasons. One is that some countries may be less rigorous with reporting, which makes the mortality rate skew higher.
In Africa, ※people with mild cases don’t bother going to a health professional and don’t get recognised as having Mpox. Whereas New Zealand, Sweden, UK, the States, it might be that a much higher proportion of people go, including those ones with very mild illness,§ he says.
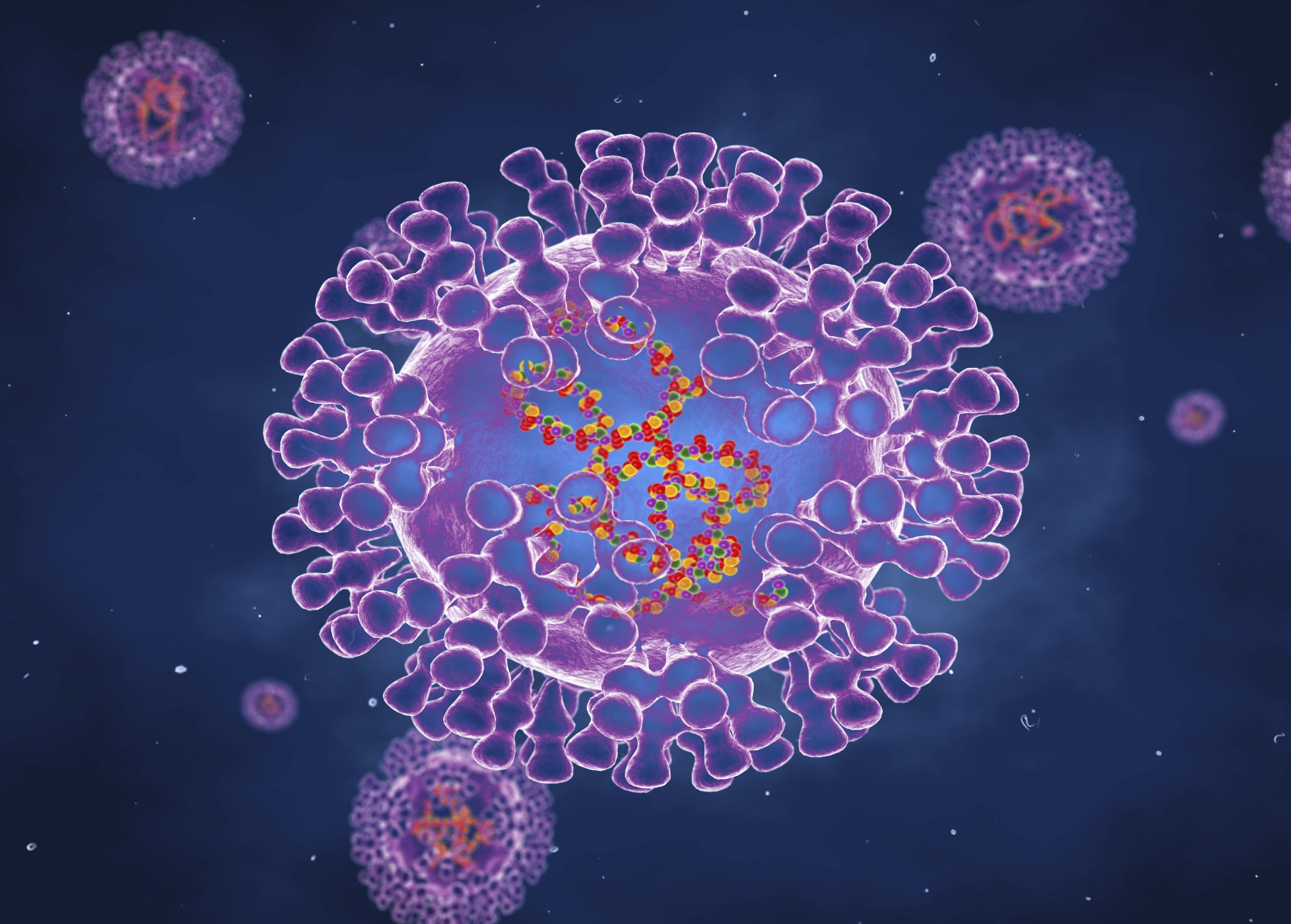
What is Mpox?

Mpox is a viral infection that’s closely related to smallpox. It used to be referred to as Monkeypox because initially scientists thought it was a virus that particularly affected monkeys.
※The first isolation of the virus was by people in Europe, who isolated it from a monkey in Europe and it had come from an African country and nobody in the laboratory had identified that virus before, so they thought this is a virus that infects monkeys,§ he says.
That initial identification proved to be false, and although it does infect monkeys Thomas says its main reservoir is rodents.
So that name is being phased out in favour of Mpox, also because people felt it was a disparaging term to associate sick people with.
Who’s most at risk?
Thomas says people with untreated HIV are most at risk. Other vulnerable people include individuals with weaker immune systems due to other health conditions or treatments, children, and the elderly.
What are the symptoms?
Thomas says it can take about a week, or even 10 days for someone to start developing symptoms. This is referred to as the incubation period.
※After about seven to 10 days they become unwell, often with a flu-like illness, with fever, aches, and pains, feeling tired, maybe off their food # nothing definitive about it, you wouldn’t necessarily know that you had Mpox at that time,§ he says.
After these symptoms appear, a person will start noticing small pox lesions. These start as small raised red bumps, develop into a blister, then scab over and fall off. That process usually takes up to two weeks.
How is it transmitted?
Mpox is transmitted through close skin-to-skin contact with someone who is infected.
Thomas says there is a risk of people transmitting the virus while they’re in the incubation period, but that it’s relatively low.
※My suspicion would be that yes it’s a contributor, but I doubt that it’s responsible for 90 percent of the cases,§ he says.
Thomas explains because the virus is transmitted mainly through skin contact, a person is most infectious when they develop the skin lesions.
How do you treat it?

There’s currently no vaccine designed to specifically treat Mpox.
But there have been a couple developed over time to treat the various kinds of pox. The latest is called JYNNEOS.
※It requires two doses of a vaccine injected into your tissues under your skin for the best protection. It gives you a dose of the virus, very similar to Mpox, not quite the same, but your immune response to that virus will protect you from Mpox,§ Thomas says.
He adds that like the Covid vaccine, this one doesn’t guarantee 100 percent immunity, it’s more around 70-80 percent. But if a person does get infected, they won’t have as severe a case of the virus.
The vaccine can also be given to people who are infected with the virus, for example close contacts who may not be showing symptoms, to avoid a severe case of Mpox.
Thomas says there won’t be a big supply of the JYNNEOS vaccine available as stock is relatively low at the moment, and advises countries that don’t have any cases to resist the urge to pre-stock, because it will take away supply from countries where the virus is most prevalent.
※I’m sure there are people in New Zealand thinking we ought to be getting in and buying as much as we can now. But I don’t think that the benefit of it being delivered to New Zealand at the moment is anywhere near the benefit that would accrue from it being delivered in the Congo.§
Check out how to listen to and follow?The Detail?here.??
You can also stay up-to-date by liking us on?Facebook?or following us on?Twitter.?